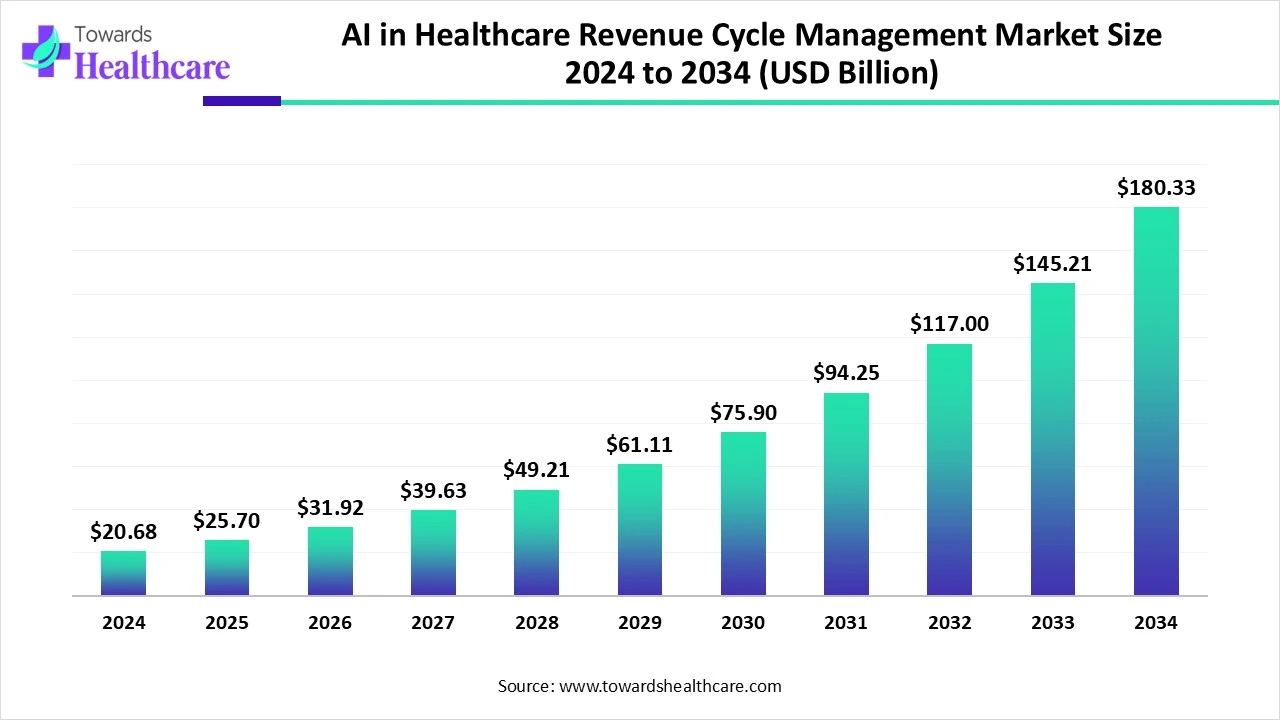
The global AI in Healthcare Revenue Cycle Management (RCM) market is experiencing a transformative boom. In 2024, the market was valued at USD 20.68 billion, and it is expected to grow to a staggering USD 180.33 billion by 2034, registering a compound annual growth rate (CAGR) of 24.20% over the forecast period from 2025 to 2034.
This remarkable growth is being fueled by a surge in demand for automation within healthcare billing, coding, claims processing, and payment systems. AI-powered RCM tools improve accuracy, reduce administrative overhead, and accelerate reimbursements, enabling healthcare providers to operate more efficiently.
Evolution of AI in Revenue Cycle Management
AI is revolutionizing the revenue cycle by automating repetitive tasks, minimizing human errors, and improving the accuracy of financial operations. From medical coding and billing error detection to claims denial prediction and collections optimization, AI technologies are streamlining once-complex workflows.
The integration of AI with electronic health records (EHRs) and cloud platforms has further accelerated the industry’s transformation. Providers are increasingly seeing improvements in cash flow, reduced costs, and enhanced decision-making through real-time data processing.
Noteworthy Innovation
In December 2024, India-based Care.fi launched RevNow, an AI-driven RCM platform designed to simplify insurance claims across the full cycle—from pre-authorization to final settlement.
Invest in Our Premium Strategic Solution: https://www.towardshealthcare.com/download-databook/5782
Key Market Trends in 2025
The industry is witnessing a rapid influx of funding and innovation:
-
In April 2025, RapidClaims raised USD 11 million to expand its AI-powered RCM platform.
-
In March 2025, R1 and Palantir partnered to launch R37, an advanced AI lab focused on improving financial performance via cutting-edge revenue cycle solutions.
Market Drivers
Increased Claim Volume and Billing Complexity
Healthcare billing is becoming increasingly complex. Manual systems often fall short when addressing payer-specific rules or coding errors, leading to revenue leakage and claim denials. AI mitigates these challenges by:
-
Analyzing large data volumes
-
Automating denial management
-
Detecting error patterns
-
Enhancing reimbursement rates
Segmental Insights
Software Segment Leads in 2024
In 2024, software accounted for the largest share of the market due to its ability to automate and scale billing and coding processes. These platforms offer:
-
Real-time analytics
-
Seamless EHR integration
-
Scalable architecture
-
Reduced administrative burden
Get All the Details in Our Solutions – Access Report Preview: https://www.towardshealthcare.com/download-sample/5782
Case in Point
In August 2024, Arsenal Capital Partners acquired Knowtion Health, enhancing its AI-driven claim resolution capabilities in the healthcare RCM space.
Rapid Growth in Services Segment
As organizations adopt AI tools, they increasingly seek professional services for implementation, optimization, and compliance. This trend is fueling the fastest growth within the services segment.
Example
In October 2024, eClinicalWorks launched a suite of AI-based RCM tools to simplify healthcare billing and boost financial efficiency.
Deployment Model Analysis
Cloud/Web-Based Platforms Dominate
Cloud-based RCM systems were the deployment model of choice in 2024. These platforms enable:
-
Real-time accessibility
-
Lower upfront investments
-
Simplified regulatory compliance
-
Reduced IT infrastructure reliance
Integrated Platforms vs. Standalone Tools
Dominance of Integrated AI-RCM Platforms
Integrated solutions lead the market due to their ability to centralize operations, improve interdepartmental coordination, and accelerate decision-making.
Standalone AI Tools Gaining Momentum
Standalone solutions, designed for specific challenges like claim denials or delayed payments, are gaining popularity for their speed of deployment and targeted functionality, especially among smaller providers.
If you have any questions, please feel free to contact us at sales@towardshealthcare.com
Regional Insights
North America Leads the Charge
North America continues to dominate the global market, driven by:
-
Advanced healthcare infrastructure
-
Early AI adoption
-
High healthcare spending
-
Strong government backing for digital transformation
United States
In January 2025, IntelligentDX introduced an AI platform to enhance EHR and EMR efficiency, addressing rising healthcare costs and billing complexities.
Canada
With a national focus on digital health innovation, Canada is investing heavily in AI tools that streamline billing, reduce denials, and support EHR integration.
Asia-Pacific: Fastest Growing Market
Asia-Pacific is poised for highest CAGR growth over the forecast period, owing to:
-
Rapid healthcare digitization
-
Rising middle-class demand
-
Increased government investment in EHRs
-
Growing use of telemedicine and insurance billing platforms
Europe’s Strategic Acceleration
Europe is advancing its AI adoption through:
-
National digitization efforts
-
Cross-border interoperability initiatives
-
Growing demand for billing accuracy and administrative efficiency
United Kingdom
The UK is boosting AI implementation through NHS digital transformation programs aimed at reducing costs and improving patient outcomes.
Germany
Germany is focusing on IT modernization, with AI solutions playing a key role in enhancing billing accuracy and easing financial operations.
Industry Highlights and Recent Developments
FinThrive’s Agentic AI Launch
In June 2025, FinThrive showcased its Agentic AI platform at the HFMA Conference. This tool uses intelligent agents to autonomously manage tasks such as prior authorizations and cash flow forecasting, significantly improving workflow optimization.
Key Acquisitions and Funding Rounds
-
In May 2025, Infinx acquired i3 Verticals’ healthcare RCM division, aiming to integrate scalable solutions and expand its service portfolio.
-
In June 2024, Adonis secured USD 31 million to scale its AI-based RCM platform compatible with over 35 EHRs and clearinghouses.
To access the full Market Report : https://www.towardshealthcare.com/price/5782