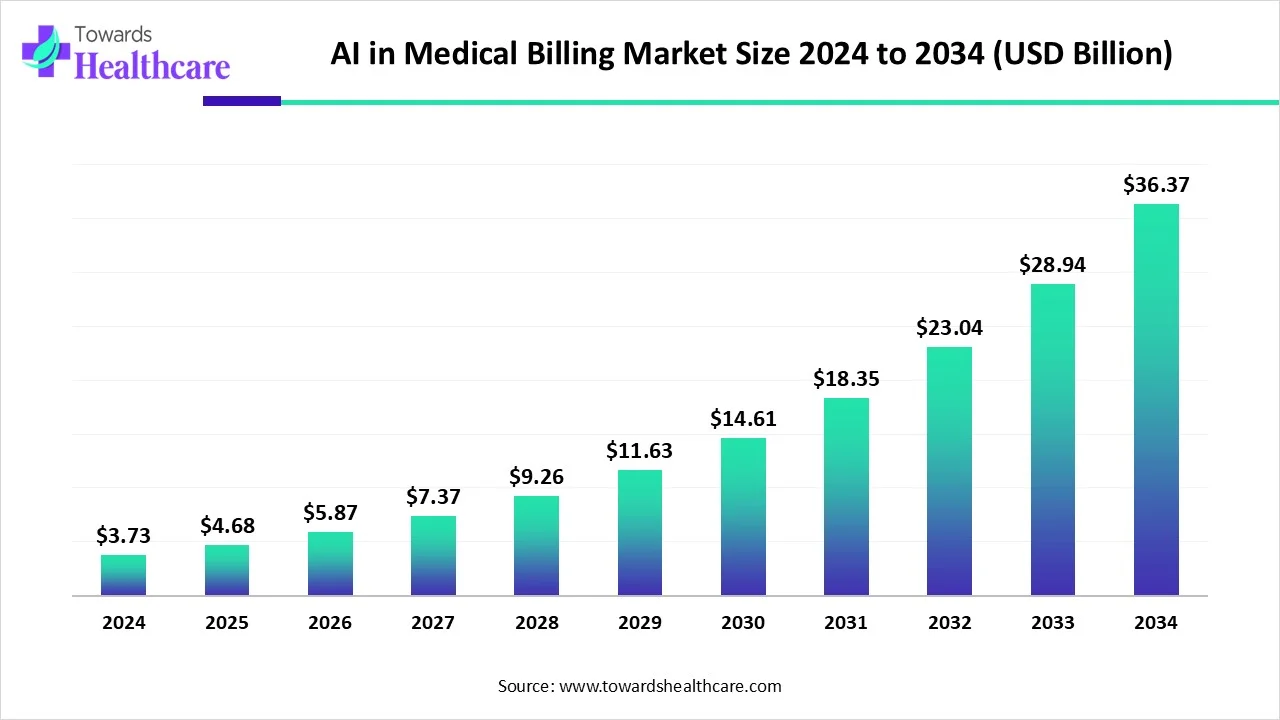
The global AI in medical billing market is undergoing a significant transformation, poised to grow from USD 3.73 billion in 2024 to an impressive USD 36.37 billion by 2034. This growth, projected at a CAGR of 25.4%, is being fueled by the widespread adoption of advanced technologies and the surge in hospital admissions worldwide.
Market Overview
AI is revolutionizing the healthcare sector, especially in administrative operations like medical billing. With the growing complexity of healthcare billing systems, AI-driven solutions are helping streamline processes, minimize human error, and ensure quicker reimbursements. These tools not only reduce administrative burdens but also enhance revenue cycle management (RCM), supporting both efficiency and compliance.
Invest in Our Premium Strategic Solution: https://www.towardshealthcare.com/download-databook/5755
Key Market Insights
-
2024 Valuation: The market is expected to cross USD 3.73 billion.
-
2034 Forecast: Anticipated to grow to USD 36.37 billion.
-
Growth Rate: Estimated CAGR of 25.4% from 2025 to 2034.
-
Regional Leadership: North America accounted for the largest revenue share in 2024.
-
Fastest-Growing Region: Asia-Pacific is set to lead in CAGR growth.
-
Leading Deployment Mode: Cloud-based solutions dominate the current market.
-
Fastest-Growing Deployment: On-premises systems expected to rise swiftly.
-
Top Application Area: Revenue cycle management led in revenue share in 2024.
-
Emerging Application Trend: Fraud detection to grow rapidly.
-
Dominant End-user: Hospitals and clinics remain the primary users.
-
High-Growth End-user: Healthcare payers are investing heavily in AI tools.
Get All the Details in Our Solutions – Access Report Preview: https://www.towardshealthcare.com/download-sample/5755
Transforming Claims Processing
AI in medical billing has become indispensable for modern healthcare systems. It allows automation of claims submission, reduces manual billing errors, tracks denials, and ensures regulatory compliance. As hospitals admit more patients due to aging populations, surgeries, and chronic illnesses, AI enables efficient billing management and personalized service offerings.
Driving Forces Behind Market Growth
Increasing Hospital Admissions
An upsurge in global hospital admissions is a major driver. Over 313 million surgeries occur annually, and the aging population is escalating healthcare needs. The United Nations projects that the population aged 65 and above will hit 2.2 billion by 2070, further intensifying the demand for automated billing systems.
Technological Advancements and Government Support
Advanced AI tools are being introduced at a fast pace. Public and private investments, along with government-backed initiatives and funding, are creating a favorable environment for AI deployment in healthcare billing.
Market Restraint: Data Privacy Concerns
Despite its potential, the adoption of AI faces hurdles. One of the critical challenges is safeguarding sensitive patient data. Privacy concerns and risks of data leakage make healthcare institutions cautious in adopting AI-powered billing systems.
If you have any questions, please feel free to contact us at sales@towardshealthcare.com
Future Outlook: EHR Integration
The future of AI in medical billing is closely linked to its integration with Electronic Health Records (EHRs). EHRs provide a centralized platform for managing patient information and automating billing tasks like insurance eligibility verification and data entry. This integration boosts claims accuracy and accelerates processing times.
Segment Analysis
Application: Revenue Cycle Management Leads
Revenue cycle management remains the largest application area. The demand for workflow optimization and competitive market dynamics encourages healthcare organizations to adopt AI billing tools. According to AKASA, 74% of healthcare entities automate parts of their revenue operations, with 46% leveraging AI.
Fraud Detection to Witness Highest Growth
The fraud detection segment is projected to expand significantly. AI helps insurers analyze vast datasets for anomalies and detect patterns linked to fraudulent claims. CMS estimates fraud losses in Medicare and Medicaid reach up to USD 60 billion annually.
End-user Insights: Hospitals Dominate, Payers to Rise
Hospitals and clinics hold the largest share, driven by high patient inflow and administrative load. Manual claim processing contributes to USD 260 billion in denied claims annually, underscoring the need for automation.
Healthcare payers, including insurance firms, are adopting AI to handle large volumes of data for verification, claims processing, and fraud prevention. This trend is expected to make payers the fastest-growing end-user segment.
Regional Highlights
North America: Technological and Infrastructural Edge
North America remains at the forefront due to the presence of leading players, favorable reimbursement policies, and advanced healthcare infrastructure. The U.S. alone recorded over 34 million hospital admissions in 2023. Organizations like Amperos Health and CollaborateMD are actively investing in AI innovation.
Asia-Pacific: Growing Awareness and Digitization
The region is experiencing rapid growth thanks to increasing awareness about insurance and healthcare digitization. China recorded over 363 million digital healthcare users in 2023, and India reported nearly 35 lakh hospital admissions in the same year. These trends highlight growing opportunities for AI adoption.
Europe: Strong Government Backing
Europe is benefiting from robust government support, favorable insurance schemes, and initiatives promoting the use of EHRs and AI. Workshops, conferences, and public-private partnerships are further fostering market expansion.
Recent Industry Developments
-
June 2025: Amperos Health launched Amanda, the first AI-powered biller, automating 75,000+ calls and recovering USD 120 million in revenue. The company secured USD 4.2 million in funding.
-
April 2025: Cedar introduced Kora, an AI voice agent for billing inquiries, capable of handling 30% of inbound calls.
-
May 2025: New Mountain Capital merged Access Healthcare, SmarterDx, and Thoughtful.ai to form Smarter Technologies.
-
February 2024: Maverick Medical AI partnered with ImagineSoftware to deploy autonomous coding solutions for enhanced operational scalability.
Industry Outlook and Conclusion
The AI in medical billing market is set to revolutionize the healthcare landscape. As hospital admissions increase and operational costs surge, AI offers scalable, error-free, and efficient billing solutions. With growing investments, advanced technologies, and increasing awareness, this market is on a trajectory of robust growth, paving the way for smarter and more accessible healthcare systems globally.
Source : https://www.towardshealthcare.com/insights/ai-in-medical-billing-market-sizing