The global nurse call systems market was USD 2.2 billion in 2024, grew to USD 2.47 billion in 2025, and is forecast to reach ~USD 6.93 billion by 2034 (CAGR 12.15% from 2025–2034), driven by aging populations, rising hospitalizations, and rapid tech integration (AI, IP, wireless).
Download the free sample and get the complete insights and forecasts report on this market @ https://www.towardshealthcare.com/download-sample/5555
Market size
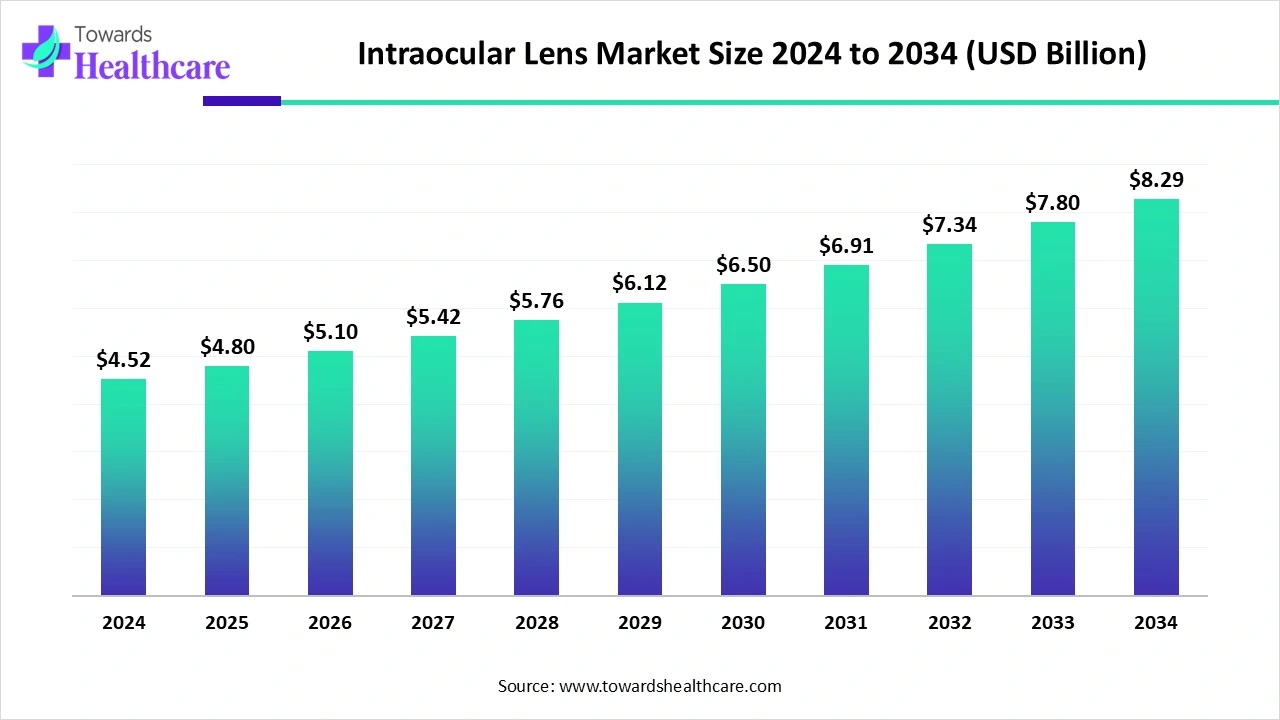
◉Base figures: USD 2.20B (2024) → USD 2.47B (2025) (reported).
◉Forecast: USD ~6.93B by 2034 (implies CAGR 12.15% between 2025–2034).
◉Technology split (2024 reported): wired ≈ USD 1.20B, wireless ≈ USD 1.00B (wired held lead in 2024).
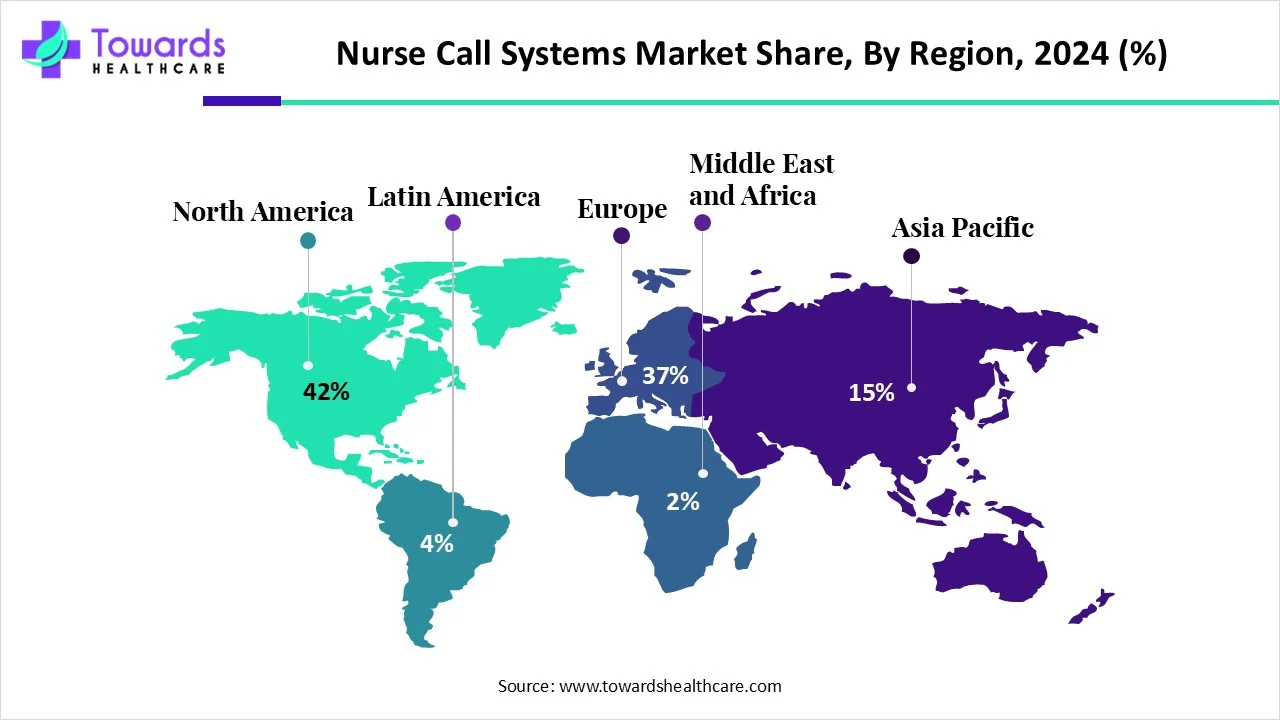
◉Regional split (2024 reported): North America USD 0.80B (≈42% market share); Europe USD 0.56B; APAC USD 0.54B; Latin America USD 0.17B; MEA USD 0.14B.
◉Technology trajectory: wired rises from 1.20B (2024) to 3.81B (2034); wireless grows from 1.00B (2024) to 3.11B (2034) — showing persistent dominance of wired in absolute terms but faster relative growth for wireless.
Type and end-use scale (2024 as anchor): integrated communication systems and hospitals are the largest buckets today; mobile systems and ASCs/clinics are the fastest-growing subsegments by rate.
Market sizing methodology note (implied by figures): combines hardware (patient stations, consoles, dome lights), software/firmware (integrations, middleware), services (installation, maintenance) and increasingly recurring software/AI services.
Market trends
◉Consolidation & M&A / strategic acquisitions: Example: Stryker’s acquisition of care.ai (Aug 2024) to expand AI and wirelessly connected medical-device portfolio — signals larger medtech players moving into nurse-call/ambient intelligence space.
◉Feature granularity & patient-centred calls: e.g., Orlando Health installed nurse-call with dedicated buttons (water, pain, toilet) to capture request-type data and prioritize workflow.
◉Integration with virtual care & AI vendors: partnerships like West-Com × VitalChat (May 2023) show convergence of nurse call, virtual visits and e-sitter/virtual care features.
◉Product launches & next-generation platforms: launches such as Ascom Telligence 7 and Fanvil Nurse Call System V1.0 Beta (Aug 2024) show emphasis on clinical workflow analytics and emergency handling.
◉Voice & ambient tech: Alexa Smart Properties collaboration (Lifeline Senior Living / Connect America, Jul 2023) highlights voice-enabled resident safety as an add-on/adjacent capability.
◉Wireless & mobile momentum: mobile systems and wireless equipment reported as fastest-growing — driven by smartphones, 5G/6G readiness and staff mobility needs.
◉Regulatory & reimbursement tailwinds: favorable policies and hospital environment mandates (e.g., CMS/OSHA references) in North America accelerate adoption for compliance and patient safety.
◉Workforce pressure & workflow optimization demand: rising nurse workloads and shortage scenarios create urgency for solutions that reduce low-value interruptions and optimize routing/response.
◉Aging population & chronic disease prevalence: demographic tailwind increases demand for wanderer control, fall detection and continuous monitoring features.
◉Cost constraint tension: high upfront costs for advanced systems remain a restraint for many low/middle-income providers — presenting an opportunity for SaaS/lease models.
AI’s role & impact of Nurse Call Systems Market
Call prioritization & triage
◉AI models analyze call metadata (time, location, patient history) + voice/text content to score urgency (e.g., “pain” vs “toilet”) and route highest-risk events first.
◉Benefit: reduces missed critical calls, improves response times for high-acuity needs.
Voice-based intent recognition & NLP
◉NLP on bedside intercoms or voice-enabled devices converts free-text/verbal patient requests into structured tasks (medication, toileting, pain).
◉Benefit: lowers false alarms and prevents unnecessary room visits; helps non-verbal or low-literacy patients communicate needs.
Prediction & proactive care
◉ML on call patterns, vitals (if integrated), and historical outcomes predicts deterioration risk or likely needs (e.g., patients who call frequently at night may need repositioning or pain reassessment).
◉Benefit: enables preemptive rounding, reducing emergent events and improving satisfaction.
Intelligent alarm filtering (alarm fatigue reduction)
◉AI clusters/filters repetitive or non-actionable alerts (e.g., repeated accidental pulls), surfaces probable false alarms, and flags genuine ones.
◉Benefit: reduces nurse desensitization and improves meaningful signal-to-noise ratio.
Workflow automation & intelligent routing
◉AI maps staffing schedules, nurse locations (RTLS), patient acuity and routes alerts to the right caregiver (charge nurse vs aide) automatically.
◉Benefit: optimizes resource allocation and decreases handoffs.
Contextual multimodal analysis
◉Combining audio, call metadata, RTLS, and EHR signals to form a richer context for automated decisions (e.g., a fall sensor + call from bathroom + older patient → highest priority).
◉Benefit: better sensitivity/specificity for critical events.
Operational analytics & capacity planning
◉Aggregate AI analytics identify bottlenecks (units with chronic high response times) and recommend staffing changes or physical layout improvements.
◉Benefit: measurable efficiency improvements and staffing ROI justification.
Personalized patient interaction
◉AI-driven suggestions for standard responses or scripts for staff or voice assistants to deliver routine instructions (e.g., “I’ll be there in 3 minutes”), improving patient perception of responsiveness.
Privacy, bias & safety considerations
◉Risks: voice/NLP models must protect PHI, avoid bias in triage scores, and be auditable. Any AI triage that influences care must have human-in-the-loop and clear fail-safes.
Monetization shift
◉AI features open SaaS/subscription revenue (analytics, predictive modules) on top of hardware sales — shifting business models to recurring revenue.
Regulatory & validation need
◉Clinical validation required for AI models that affect prioritization; potential regulatory oversight (depending on jurisdiction) if algorithms affect clinical decisions.
Regional Insights of Nurse Call Systems Market
North America
Market Leadership
◉Accounts for 42% of the global market in 2024 (USD 0.80 billion).
◉The U.S. leads the region, followed by Canada, due to advanced hospital networks.
Key Growth Drivers
Large Hospital Base & Stringent Regulations
◉The U.S. has one of the world’s largest clusters of acute-care hospitals.
◉Regulatory oversight from CMS, OSHA, and Joint Commission mandates communication and safety systems.
Funding & Reimbursement Policies
◉Federal and state-level funding allocated to hospital IT modernization.
◉Reimbursement models emphasize improved patient outcomes, incentivizing hospitals to adopt real-time communication systems.
Strong Healthcare IT Spending
◉Per-capita spending on healthcare IT in North America surpasses Europe and Asia-Pacific.
◉Supports faster adoption of digital nurse call and integrated platforms.
Technology Trends
Integrated & IP-based Nurse Call Systems
◉Rapid shift from legacy wired models to IP-enabled systems.
◉These allow integration with hospital networks, mobile devices, and centralized command centers.
AI & Real-Time Location Systems (RTLS)
◉AI is used for predictive alerts, workload management, and workflow automation.
◉RTLS tracks staff, patients, and equipment to optimize resource allocation.
◉Example: Hill-Rom piloting High Precision Locating (HPL) solutions.
Competitive Landscape
Dominance of Established Vendors
◉Stryker, Hill-Rom, Rauland-Borg, and Ascom dominate the market.
M&A and Partnerships
◉Example: Stryker’s acquisition of care.ai to integrate ambient intelligence into nurse call solutions.
Challenges
Lengthy Procurement Cycles
◉Hospitals operate on 3–7 year budget cycles, delaying adoption.
Interoperability Demands
◉New systems must integrate with existing legacy platforms, which increases complexity.
Europe
Market Position
◉Second-largest regional market after North America.
◉Strong adoption in Western Europe, with Germany, France, and the U.K. as key hubs.
Key Growth Drivers
National Digitization Programs
◉EU-wide initiatives for digital health infrastructure.
◉Germany’s Digital Act (March 2024) mandates communication digitization in hospitals and long-term care.
Healthcare Workforce Challenges
◉Europe faces a persistent shortage of nurses and medical staff.
◉Nurse call systems reduce staff workload and support safer patient monitoring.
Technology Trends
Preference for Integrated Communication Platforms
◉Hospitals prefer solutions that centralize alarms, staff communication, and patient requests.
Adoption Momentum in Germany
◉Regulatory push creates demand for advanced nurse call and hospital communication systems.
Compliance with Interoperability Standards
◉Emphasis on open standards to ensure integration with EHR and telehealth platforms.
Opportunities
Cross-border Collaboration
◉Vendors can leverage EU frameworks for multi-country rollouts.
Integration with Telehealth
◉Potential to embed nurse call with virtual consultations and digital monitoring systems.
Challenges
Fragmented Healthcare Systems
◉Each country has unique procurement and regulatory requirements.
Budget Constraints in Eastern Europe
◉Lower adoption due to limited capital investment in hospitals.
Asia-Pacific
Market Growth
◉Fastest-growing region, expanding at double-digit CAGR.
◉Market size in 2024: USD 0.54 billion, expected to surpass Europe by 2030.
Key Growth Drivers
Healthcare Infrastructure Expansion
◉Massive hospital construction and modernization in China, India, and Southeast Asia.
◉Governments allocating funds for hospital digitization.
Demographic Shifts
◉Aging population in Japan, South Korea, and China increasing demand for long-term and acute care.
◉Rising chronic diseases creating higher inpatient volumes.
Medical Tourism
◉Countries like Thailand, Singapore, and India developing advanced private hospitals to attract global patients.
Country-Specific Highlights
China
◉Government-led push for digital health ecosystems.
◉Nurse call systems integrated into national smart hospital frameworks.
India
◉70,000 hospitals across urban and rural areas.
◉Strong procurement momentum — >300 nurse call tenders published by April 2025.
Japan & South Korea
◉Rapid adoption of wireless nurse call systems in elder care facilities.
Technology Trends
Wireless & Mobile Solutions
◉Preferred due to cost-effectiveness, scalability, and ease of installation.
Localized Customization
◉Vendors adapting systems to local languages and cultural needs.
Opportunities
Low-cost Wireless Models
◉Huge potential in India, Indonesia, and rural China.
Government Partnerships
◉Public-private collaborations in digital health projects.
Challenges
High Price Sensitivity
◉Hospitals in emerging markets often demand budget-friendly solutions.
Regulatory Diversity
◉Lack of harmonized standards across countries slows multinational rollouts.
Latin America
Market Position
◉Smaller compared to North America, Europe, and Asia-Pacific, but growing steadily.
◉Brazil and Mexico are leading markets.
Key Growth Drivers
Urban Healthcare Expansion
◉New hospitals in metropolitan cities drive demand.
Private Healthcare Investment
◉Private hospital chains are investing in modern communication systems to differentiate themselves.
Challenges
Budgetary Limitations
◉Public hospitals operate under restricted budgets, slowing large-scale adoption.
Technology Refresh Delays
◉Many facilities extend the use of outdated systems.
Opportunities
Wireless Deployment
◉Cost-effective wireless models appeal to mid-sized hospitals.
Service-based Business Models
◉Managed services or leasing models can increase affordability.
Middle East & Africa
Market Position
◉Smallest market share but high growth potential in select countries.
Major adoption in Gulf Cooperation Council (GCC) countries; slower in Africa.
Key Growth Drivers
High-Spend Gulf Economies
◉Saudi Arabia, UAE, and Qatar investing heavily in mega-hospital projects.
Private Hospital Development
◉Ambitious plans for luxury and specialized hospitals to attract medical tourism.
Challenges
Market Fragmentation
◉Stark contrast between advanced Gulf hospitals and underfunded African facilities.
Localization Needs
◉Vendors often need regional partners for regulatory compliance and cultural adaptation.
Opportunities
Premium Systems in Gulf
◉High demand for advanced, integrated platforms in Saudi Arabia and UAE.
Affordable Solutions in Africa
◉Wireless and mobile systems can address low-resource environments.